-
How Changing Your Lifestyle Can Help Control and Avoid Varicose Veins
How Changing Your Lifestyle Can Help Control & Avoid Varicose Veins
Varicose veins are a common issue that many people face as they get older, particularly in Sugar Land, TX. These swollen, twisted veins can appear in various parts of the body, though they are most commonly found in the legs. While varicose veins are not usually life-threatening, they can cause discomfort, pain, and embarrassment. Thankfully, lifestyle changes can help manage, control, and even prevent the development of varicose veins.

Understanding Varicose Veins
Varicose veins occur when the veins in your legs become enlarged and twisted. This happens when the valves inside the veins become weak or damaged, causing blood to pool and the veins to bulge out. The result is visible, often swollen veins that can be painful or unsightly.
Some people are more prone to developing varicose veins due to factors such as age, genetics, pregnancy, and prolonged standing or sitting. While varicose veins are more common in women, they can affect anyone. There are also many different varicose veins symptoms and varicose veins causes.
The Role of Lifestyle in Varicose Veins
Your lifestyle plays a significant role in both the prevention and management of varicose veins. While you can’t change some risk factors like age or genetics, there are many steps you can take to reduce your risk and alleviate symptoms if you already have varicose veins. Here are some ways your daily habits and routines impact varicose veins:
- Inactivity: Prolonged sitting or standing can cause blood to pool in your legs, increasing the likelihood of varicose veins.
- Obesity: Carrying extra weight puts added pressure on your veins, which can contribute to the development of varicose veins.
- Diet: Poor dietary habits can affect your circulation and vascular health, while a diet high in salt and low in fiber can increase the risk of varicose veins.
- Smoking: Smoking damages the blood vessels, contributing to poor circulation and increasing the risk of vein-related problems.
Effective Lifestyle Changes to Control & Prevent Varicose Veins
Making certain lifestyle changes can help prevent the development of varicose veins or prevent existing ones from worsening. Instead of needing professional varicose vein treatment, you may benefit from:
- Exercise regularly: Physical activity is one of the best ways to improve circulation and strengthen the muscles that support your veins. Walking, swimming, or cycling are particularly effective in reducing the risk of varicose veins.
- Maintain a healthy weight: Losing excess weight helps reduce pressure on your veins, lowering your chances of developing varicose veins.
- Elevate your legs: To improve circulation, try elevating your legs above your heart level for 15-20 minutes a few times a day. This can help alleviate pressure and prevent blood from pooling in your veins.
- Wear compression stockings: Compression stockings help improve blood flow by applying gentle pressure to your legs. This can reduce swelling and pain caused by varicose veins.
- Avoid prolonged standing or sitting: If you have a job that requires long periods of standing or sitting, make sure to take breaks and move around. Stretching your legs or walking for a few minutes every hour can keep your blood flowing and reduce the risk of varicose veins.
Additional Tips for Vein Health
In addition to the lifestyle changes mentioned above, here are some extra tips to improve your vein health:
- Stay hydrated: Drinking plenty of water helps maintain healthy circulation, preventing your veins from becoming overly stressed.
- Eat a balanced diet: A healthy diet rich in fiber, vitamins, and minerals can support your blood vessel health. Focus on foods that are high in antioxidants and omega-3 fatty acids to promote circulation.
- Limit alcohol consumption: Excessive drinking can weaken blood vessel walls, contributing to varicose veins. Stick to moderate alcohol intake to maintain healthy circulation.
- Don’t cross your legs: Crossing your legs while sitting can restrict blood flow and lead to increased pressure on your veins. Try to sit with your feet flat on the floor to improve circulation.
When to Seek Medical Advice
If your varicose veins are causing significant pain, discomfort, or swelling, or if you notice changes in the appearance of your veins, it’s important to seek medical advice. While varicose veins are typically not dangerous, they can sometimes lead to complications such as blood clots or ulcers.
Contact Reddy Cardiac Wellness and Diabetes Reversal Center in Sugar Land, TX, if you are concerned about your varicose veins. A healthcare professional can evaluate your condition and recommend appropriate treatment options, including minimally invasive procedures or varicose vein surgery if necessary.
Take Control of Your Vein Health
While varicose veins may be a common issue, they don’t have to control your life. By making simple changes to your lifestyle, you can significantly reduce your risk and keep your veins healthy. Exercise, healthy eating, and taking care of your circulation can go a long way in preventing varicose veins and alleviating symptoms. Take control of your vein health today by adopting these lifestyle changes and reaching out to a professional if needed. Contact Reddy Cardiac Wellness and Diabetes Reversal Center today to get personalized support and expert care for your vein health.
-
How Stress and Heart Palpitations Are Related
Why Stress Causes Heart Palpitations and How You Can Control It
Heart palpitations can be a concerning experience, especially when they seem to appear out of nowhere. In Sugar Land, TX, many people find themselves struggling with palpitations tied to stress or anxiety. These sensations can feel like your heart is racing, fluttering, or skipping beats, and they often occur during times of high emotional pressure. The good news? Stress-related heart palpitations are common and can be managed with the right strategies.

What Are Heart Palpitations?
Heart palpitations are the feeling of your heart pounding, fluttering, or beating irregularly. They can happen at any time, even when you’re sitting still or lying down. While they’re often associated with anxiety or stress, palpitations can also be triggered by physical exertion, caffeine, medications, or certain medical conditions. However, in many cases, emotional triggers such as stress and anxiety are the primary causes.
The feeling of heart palpitations is not always a sign of a serious problem, but they can be uncomfortable and worrying. Understanding the connection between stress and palpitations can help you reduce your symptoms and take control of your health.
Common Causes, Including Emotional Triggers
While heart palpitations can have a variety of causes, emotional triggers play a significant role. Here are some of the most common factors:
- Stress: Physical and emotional stress can cause your heart rate to increase, leading to palpitations.
- Anxiety: Anxiety disorders often cause episodes of racing heartbeats, especially when feeling overwhelmed or fearful.
- Caffeine or stimulants: These substances can trigger palpitations by stimulating the nervous system. Sugar heart palpitations can sometimes occur.
- Hormonal changes: Pregnancy, menopause, or thyroid issues can contribute to heart palpitations.
- Dehydration or low blood sugar: Both conditions can cause your heart to work harder, resulting in palpitations.
How Stress Affects the Heart
When you’re stressed, your body releases hormones like adrenaline and cortisol that prepare you to react to danger. This is known as the “fight or flight” response. These hormones increase your heart rate, tighten your blood vessels, and elevate blood pressure, which can lead to the sensation of palpitations.
While stress is a natural response to challenging situations, chronic stress can have a long-term impact on your heart. Over time, persistent high stress levels can contribute to heart disease, high blood pressure, and other cardiovascular issues. Stress management is therefore essential for both your mental and physical health.
Signs Your Palpitations May Be Stress-Related
If your palpitations are stress-related, they often have specific characteristics. While there are many potential heart palpitations causes, stress can often be a factor. Here’s what to watch for:
- You notice palpitations during or after stressful events.
- They’re accompanied by feelings of anxiety, nervousness, or tension.
- The palpitations are irregular but not painful.
- You experience other stress symptoms such as sweating, shaking, or difficulty relaxing.
- The palpitations subside once the stressor is resolved.
When to Be Concerned
While occasional heart palpitations are typically not a cause for concern, there are certain situations where you should seek medical help. If your palpitations are frequent, severe, or accompanied by any of the following, it’s important to talk to a healthcare provider:
- Chest pain or discomfort
- Shortness of breath or dizziness
- Fainting or lightheadedness
- Swelling in the legs or ankles
- A history of heart disease
Managing Stress to Reduce Heart Palpitations
There are several strategies you can implement to manage stress and reduce the frequency of heart palpitations:
- Relaxation techniques: Practices like deep breathing, meditation, and yoga can help activate your body’s relaxation response.
- Exercise: Regular physical activity reduces stress and strengthens the heart.
- Sleep hygiene: Aim for at least 7-8 hours of sleep each night to help your body recover and manage stress better.
- Mindfulness: Mindfulness practices can help you stay present and reduce stress by preventing you from dwelling on worries.
- Talking to a professional: Speaking with a therapist can help address underlying anxiety or stress issues contributing to palpitations.
Treatment Options
In some cases, you may need additional support to manage heart palpitations. These heart palpitation treatment options can include:
- Medications: Anti-anxiety medications or beta-blockers may be prescribed to help regulate your heart rate and manage anxiety.
- Cognitive-behavioral therapy (CBT): CBT is effective in helping people reduce stress and anxiety that contribute to heart palpitations.
- Biofeedback: This technique teaches you how to control certain bodily functions, including heart rate, to reduce stress.
Take Control of Your Heart Health
Stress and heart palpitations can be unsettling, but with the right tools and support, you can manage your symptoms. If you’re experiencing frequent palpitations and stress in Sugar Land, TX, don’t hesitate to reach out to Reddy Cardiac Wellness and Diabetes Reversal Center. We can help you discover the best heart valve disease treatment option. Acting now can help you regain control over your health and well-being. Contact us today to schedule a consultation.
-
How to Deal with Anxiety’s Contribution to Shortness of Breath
How Anxiety Impacts Breathing and Effective Ways to Find Relief
Feeling like you can’t catch your breath can be incredibly unsettling, especially if you’re not sure what’s causing it. In Sugar Land, TX, many people dealing with anxiety experience this frightening sensation. Anxiety-induced shortness of breath is a common yet often misunderstood condition that can make it difficult to go about your day. The good news? It’s manageable—and you’re not alone.

Understanding the Connection Between Anxiety & Shortness of Breath
Anxiety impacts both the mind and body. When your brain perceives a threat—real or imagined—it signals your body to prepare for “fight or flight.” This response includes a flood of stress hormones that increase heart rate, tense muscles, and alter your breathing pattern. You may not even realize your breathing has changed until you feel lightheaded or tight in the chest.
This chain reaction is what often leads to anxiety and shortness of breath. The sensation can be alarming and mimic more serious conditions, but understanding the link between mental health and breathing issues is the first step in taking control.
Why Anxiety Causes Breathing Issues
When anxiety hits, your breathing often becomes shallow and rapid. This is known as hyperventilation. It throws off the balance of oxygen and carbon dioxide in your bloodstream, causing symptoms like dizziness, tingling in the fingers, and, yes, shortness of breath.
In some cases, the anxiety may also trigger chest tightness or a feeling of heart fluttering. These symptoms can mimic cardiac issues, which only fuels the fear and intensifies the anxiety, creating a vicious cycle.
It’s important to understand that while these symptoms feel physical, their root cause is often emotional or psychological. This doesn’t mean they’re “all in your head”—it means the body is responding to stress in a very real way.
Common Symptoms to Watch For
If you’re trying to determine whether your breathing difficulties are related to anxiety, here are some signs to look for:
- You feel short of breath but are still able to speak in full sentences
- Symptoms appear during or shortly after stressful situations
- You notice a fluttering sensation in your chest or rapid heartbeat
- There’s no obvious physical cause like exercise or illness
- Breathing difficulty comes and goes depending on your emotional state
Quick Relief Techniques for Anxiety-Related Shortness of Breath
There are a few immediate techniques that can help manage anxiety-induced shortness of breath when it strikes:
- Pursed-lip breathing: Inhale through your nose and exhale slowly through pursed lips. This slows your breathing and helps restore proper oxygen levels.
- 4-7-8 technique: Inhale for 4 seconds, hold for 7, and exhale for 8. Repeat until your breathing steadies.
- Grounding exercises: Focus on what you can see, hear, touch, smell, and taste to anchor yourself in the present.
- Progressive muscle relaxation: Tense and release muscles throughout your body, starting with your toes and working up to your face.
When to Seek Professional Help
You don’t have to manage anxiety or shortness of breath alone. While many find relief with at-home techniques, others benefit from professional support. If symptoms are frequent, intense, or interfere with your daily life, it’s time to consult with a doctor or mental health professional.
A medical provider can rule out other shortness of breath causes such as asthma, heart valve disease, or other cardiovascular concerns. Once a proper diagnosis is made, you can explore shortness of breath treatment options that address both the physical and emotional components.
Take Control of Anxiety & Your Breathing
Anxiety can feel like it’s taking over, but you have more control than you might think. With the right tools and support, you can manage your symptoms and take a deep breath—literally and figuratively. If you’re in the Sugar Land, TX area and want help addressing anxiety, shortness of breath, or related heart symptoms, Reddy Cardiac Wellness and Diabetes Reversal Center is here to help. Contact us today to schedule a consultation and start your journey to better health.
-
The Root Causes of Heart Failure
Understanding the Root Causes of Heart Failure and How to Manage It
Heart health is essential for your overall well-being, so you should make every effort to ensure yours is in peak condition. If you live in Sugar Land, TX, Reddy Cardiology can help you do that and prevent heart failure. We specialize in cardiac wellness and provide personalized care to improve heart health for our patients from throughout the region. Our expert cardiologists have years of experience treating cardiac conditions with compassion and precision. With that in mind, read further to understand what heart failure is, the common root causes, key risk factors, symptoms, and potential treatments.

What Is Heart Failure?
Heart failure doesn’t mean that your heart has stopped working altogether. It’s a condition where your heart isn’t pumping blood as efficiently as it should. When this happens, your organs and tissues may not get enough oxygen-rich blood, leading to fatigue, shortness of breath, and other complications. Heart failure is a chronic condition. While it cannot always be cured, a trusted cardiologist can help you manage it effectively through a combination of lifestyle changes and medical treatment.
Common Heart Failure Causes
Understanding the causes of heart failure can help you reduce your risk and maintain a healthier heart. Below are some of the most common contributing factors:
- Coronary Artery Disease (CAD) – This occurs when the arteries that supply blood to the heart narrow or become blocked, reducing blood flow and straining the heart.
- High Blood Pressure – When your blood pressure is too high, your heart must work harder to pump blood, which can weaken it over time.
- Diabetes – High blood sugar levels can damage your blood vessels and heart tissue, increasing the risk of heart failure.
- Heart Valve Disease – Improperly functioning heart valves may cause the heart to work harder, leading to strain.
- Heart Attack History – A previous heart attack can scar the heart muscle, affecting its ability to pump effectively.
Be Wary of Heart Failure Risk Factors
Certain lifestyle choices and medical conditions can increase your risk of developing heart failure. Recognizing these common risk factors early is key to protecting your heart:
- Obesity – Excess weight adds strain on the heart and contributes to conditions like high blood pressure and diabetes.
- Smoking – Smoking damages both the heart and blood vessels, significantly raising your risk.
- Family History – Genetics can play a role, especially if close family members have heart disease.
- Sedentary Lifestyle – A lack of physical activity can contribute to weight gain and poor cardiovascular health.
- Poor Diet – Diets high in saturated fats, sodium, and sugar can lead to clogged arteries and other heart problems.
How to Prevent Heart Failure and Maintain Your Health
Prevention is often the best treatment. Taking proactive steps to support your health can significantly lower your risk of heart failure. Here are ways you can get started:
- Adopt a Heart-Healthy Diet – Focus on eating fruits, vegetables, whole grains, lean proteins, and healthy fats like those found in fish and nuts.
- Stay Active – Aim for at least 150 minutes of moderate exercise each week, like brisk walking or swimming.
- Quit Smoking – Seek support and resources to help you quit smoking for good.
- Manage Stress – Practice relaxation techniques like deep breathing, meditation, or yoga to reduce stress levels.
- Schedule Regular Check-Ups – Visit your doctor for routine check-ups to monitor your blood pressure, cholesterol levels, and blood sugar.
Identifying Heart Failure Symptoms
Recognizing heart failure symptoms can make a significant difference when seeking medical care. If you or a loved one experiences the following common heart failure symptoms, consult a cardiologist or healthcare provider right away:
- Shortness of breath during activities or even while resting
- Persistent fatigue or weakness
- Swelling in the legs, ankles, or feet
- Rapid or irregular heartbeat
- Difficulty concentrating or confusion
- Persistent coughing or wheezing, sometimes with pink, frothy mucus
Potential Heart Failure Treatments
If you’re diagnosed with heart failure, Reddy Cardiology can recommend multiple methods of managing symptoms and improving your quality of life. We personalize all of our treatments, so working closely with our cardiovascular team is essential. Heart failure treatments may include one or more of the following:
- Lifestyle Changes – We may recommend diet adjustments, tailored physical activity routines, and smoking cessation.
- Medications – Certain medications – such as diuretics, ACE inhibitors, and beta-blockers – help manage blood pressure, reduce fluid buildup, and support the heart’s function.
- Cardiac Interventional Procedures – Advanced procedures like angioplasty or valve repair may be necessary if structural issues contribute to heart failure.
- Implantable Devices – Devices like pacemakers or defibrillators can help stabilize irregular heart rhythms.
What to Do if You Experience Serious Heart Problems
If you suspect you’re experiencing a cardiac emergency, such as chest pain, fainting, or severe shortness of breath, seek immediate medical attention. It’s important not to delay care. For non-emergency concerns, schedule an appointment with a cardiologist to assess your condition and develop an appropriate treatment plan.
Reddy Cardiology Can Be Your Lifeline
Reddy Cardiology is committed to helping you maintain a strong heart and a healthy life. Our team is experienced in diagnosing and treating heart failure, as well as guiding patients through preventative strategies. We understand every patient’s needs are unique, so we offer personalized care plans. From state-of-the-art cardiac interventional procedures to compassionate patient care, we’re here to support every step of your heart health journey.
Contact Us for Cardiac Wellness Care in Sugar Land, TX, Today
Put your heart in expert hands. If you need guidance regarding heart failure symptoms, treatments, or prevention tips, Reddy Cardiology in Sugar Land, TX, is the team to call. With our expertise and your commitment, better heart health is within reach. Contact us today to schedule an appointment and begin your cardiac wellness journey.
-
One condition may be causing most of our medical problems including obesity and doctors may not know how to treat it
With all the medical problems we see today including diabetes, heart disease, obesity, and some cancers; one very common condition may be fueling most of these diseases. This disease is called Non-Alcoholic Fatty Liver Disease or more simply ‘FATTY LIVER’. It is seen in people who don’t drink alcohol, but their livers resemble that of a person who is an alcoholic. This condition is more common than you might think; in fact 25% of people in the United States are affected by it and probably, even more, are undiagnosed. So there’s a good chance you might have it. The worst part is many doctors do not know how to treat this disease, let alone check for it routinely.
Have you heard the saying “All roads lead to Rome”? It is an old idiomatic expression which explains that many different routes would lead to the same goal. It is based on the fact that the Roman Empire’s road system is designed in such a way that all of its roads radiate from one source which is the capital. Fatty liver disease is exactly like Rome. Most if not all disease processes emanate from fatty liver.
So if you have diabetes, heart disease, obesity, or other diseases, you also have a fatty liver. And the only way to cure all these conditions is to reverse your fatty liver.
Let’s take a crack at it today and learn everything about fatty liver disease and how to reverse it. Watch the video.
-
Two of the Common Things You Complain Every Day May Be a Sign of an Already Advanced Disease
As simple and as common as forgetting where you placed your keys and feeling tired most of the time could be the only indications that a silent disease is on its advanced stage.
I have been in practice for eighteen years in the field of Cardiology and as I look at all the medical conditions like heart disease, diabetes, and obesity in a different perspective, I now realize that they all stem from a condition called Fatty Liver Disease. One day I was talking to my friend who is a gastroenterologist and I asked him a simple question; if I have a fatty liver, what signs and symptoms would I have? He said, ‘None.’ So I asked him again, if I continue to develop fatty liver to the point where all of my liver cells are full of fat, what would happen then? He told me, ‘You will develop inflammations in your liver which will lead to fibrosis or ‘scarring’ of the liver. But then you will still have no symptoms. Even if ninety percent of your liver is scarred, you will still have no symptoms. The only time you may have symptoms is when ninety-five percent of the liver is already scarred. But most people, even at this stage, will only have two symptoms; one is mild memory loss and the other is mild fatigue.’
Now, who among you have never experienced forgetting where you placed your keys and feeling tired all the time? The scariest thing is that when you are at this point, you are just one step closer to liver cirrhosis and liver failure. More than ninety percent of your liver could be scarred and you may never know it until it is too late.
Watch the video below and learn everything you can about fatty liver disease and how it can be diagnosed. Find out which test will tell you how much ‘fat’ or ‘scar’ is in your liver and work on reversing Fatty Liver Disease.
-
Introducing FibroScan, A New Diagnostic Tool to Accurately Detect Fatty Liver Disease and Eliminate the Need for a Painful Liver Biopsy
Non-Alcoholic Fatty Liver Disease (NAFLD) is the leading cause of chronic liver disease and is now projected to become the leading cause of liver transplants within the next decade. Fatty liver disease develops silently and signs and symptoms become obvious only when it becomes irreversible. Most people who die of the disease don’t realize they have it until the very late stage. Therefore screening people with risk factors of liver disease is critical in catching the disease early.
Reddy Cardiac Wellness and Diabetes Reversal Center of Sugar Land, Texas is announcing the availability of FibroScan, a newly approved technology to accurately and painlessly diagnose liver disease. FibroScan is an ultrasound-based vibration-controlled transient elastography (VCTE) device used to asses liver elasticity for the detection of significant fibrosis and for the diagnosis of cirrhosis in hepatitis C virus, hepatitis B virus, biliary liver disease, alcoholic liver disease, and non-alcoholic fatty liver disease.
A FibroScan test eliminates the need for a liver biopsy, where a 6-inch needle is inserted into the liver to extract a sample for testing under a microscope. In addition to being painful, biopsies are expensive, running as high as $7,000. FibroScan tests are dramatically less expensive.
FibroScan was first introduced in Europe in 2003 and received clearance by the US Food and Drug Administration (FDA) in April 2013. Now, FibroScan has a newly developed controlled attenuation parameter (CAP) that detects and quantifies steatosis, the fatty accumulations in the liver cells. It can precisely tell you how much fat is in your liver.
As of now, the Reddy Cardiac Wellness and Diabetes Reversal Center is the only center in the state of Texas that has the CAP capability in their FibroScan machine. The population of the greater Houston area can surely take advantage of this technology to have their livers checked for the silent fatty liver disease.
The American Liver Foundation estimates that 1 in 10 Americans has liver disease. Liver disease is the fourth leading cause of death among adults 45-54. More than 6 million children in the U.S. have non-alcoholic fatty liver disease and the wrongful diet most Americans eat could be to blame.
People with fatty liver can develop a more serious form of fatty liver called steatohepatitis in which the fat causes inflammation that leads to fibrosis or ‘scarring’ of the liver. Once the liver is replaced with scar tissues, it will develop cirrhosis and liver failure. This is the only time you will have signs and symptoms. By then it could be too late. The only way to prolong life at this point is to have a liver transplant. But the most important questions to ask are: who are you going to ask for a liver and how sure are you that the donor’s liver you are getting is healthy?
-
What Is In Your Liver: Fat or Scars?
FibroScan is an ultrasound-based vibration-controlled transient elastography (VCTE) device used to assess liver elasticity for the detection of significant fibrosis and for the diagnosis of cirrhosis in hepatitis C virus, hepatitis B virus, biliary liver disease, alcoholic liver disease, and non-alcoholic fatty liver disease. FibroScan also has a newly developed controlled attenuation parameter (CAP) that detects and quantifies steatosis, the fatty accumulations in the liver cells. It can precisely tell you how much fat is in your liver.
If you want to find out if your liver has fat or scars, you have two choices. You can either undergo a painful procedure called a ‘liver biopsy’ or do a simple FibroScan test which is painless. In addition to being painful, biopsies are expensive, running as high as $7,000. FibroScan test eliminates the need for a liver biopsy and is far less expensive.
FibroScan test is now available at the Reddy Cardiac Wellness and Diabetes Reversal Center in Sugar Land, Texas. The population of the greater Houston area can surely take advantage of this technology to have their livers checked for liver disease.
By doing a FibroScan test in our facility, we will accurately tell you how much fat is in your liver and if you are developing scars in your liver. These scars, if left untreated, will lead to cirrhosis and death unless you get a liver transplant. But why would you want to wait for that to happen? Find out today if you have fat and scars in your liver and let us teach you how you can reverse this disease.
Watch the video.
-
Can Type 2 (Adult-Onset) Diabetes Be Reversed?
The idea of completely reversing diabetes has been questioned time and time again. In order to determine the answer to this question, you must take into account a few factors, such as what type of diabetes are you dealing with and whether or not your body is producing insulin. There are two types of diabetes, type 1 and type 2. Type 1 or sometimes called juvenile-onset diabetes is rare and usually diagnosed in children and young adults, though it can develop at any age. In type 1 diabetes, the body does not produce insulin.
Insulin is a hormone that helps your body’s cells use sugar, or glucose, as fuel for their functions. If you do not have insulin, you may develop hyperglycemia (high blood sugar), which can cause long-term complications if the blood sugar levels stay elevated for long periods of time. Type 1 diabetes cannot be reversed and people with this type of diabetes need life-long insulin therapy. However, keeping a healthy diet and regular exercise can reduce the amount of insulin needed to maintain a normal blood sugar level.
Type 2 or adult-onset diabetes is the most common form of diabetes. In type 2 diabetes, the body produces insulin but the body is resistant to its effect, therefore making it hard to maintain a normal blood sugar level. Often a medication called metformin is prescribed to help restore the body’s proper response to insulin. Other medications may also be added to help reduce the amount of blood sugar in the body.
Insulin resistance is caused by a diet high in fructose, being overweight, and lack of physical activity. If you make improvements on your diet and you lose a significant amount of weight, you can reverse insulin resistance and make your body sensitive to insulin again, even without medications. By reversing insulin resistance, you also reverse type 2 diabetes.
Typically, doctors refer to “diabetes reversal” when you are able to go off your medication while engaging in a healthy lifestyle program. Obviously, when you are not taking medication for diabetes and your blood sugar is under control, you do not have diabetes or you have reversed diabetes. But the important message here is that you have to keep a healthy lifestyle program. If you fall off the wagon and start eating the wrong stuff again and stop exercising, you will end up with diabetes yet again.
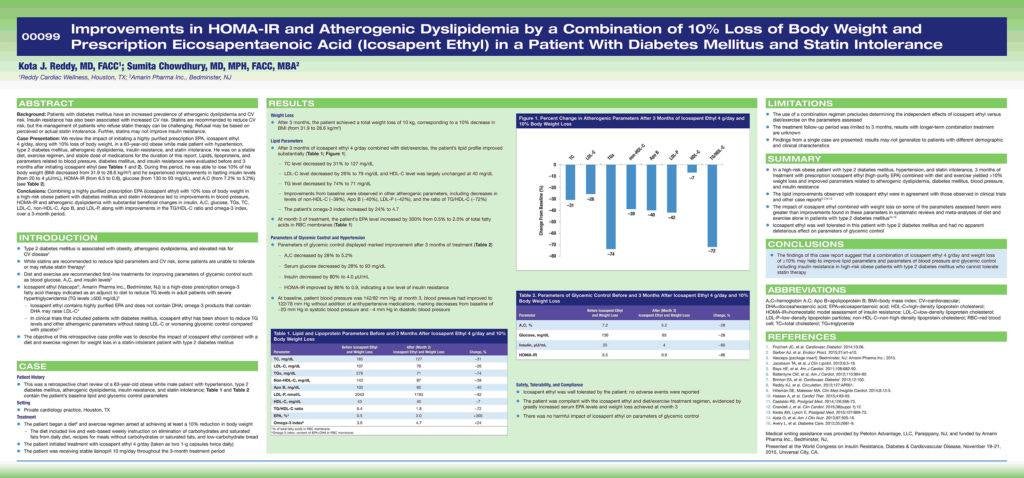
So, to answer the question ‘Can type 2 (adult-onset) diabetes be reversed?’, the answer is YES. Can it be reversed with diet and exercise? Absolutely YES. Watch the video and learn about the case of a 63 y/o Caucasian male who reversed his type 2 diabetes in 90 days after joining our program. This case report was presented at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease on November 19–21, 2015 at Universal City, CA.
-
This Combination of Carbohydrate and Fat is the Reason Why Heart Attacks are Rampant During the Holidays
There is a 40% increase of heart attacks in the last two weeks of December and first two weeks of January because of what we eat most during the holidays. The combination of sugar and fat, especially the ‘caramelized’ fat seen in almost all desserts can make the small-sized bad cholesterol ‘oxidized’ to form plaques faster or make existing plaques unstable and cause heart attacks.